Trio of papers examines the complexity of handoffs and strategies to improve them.
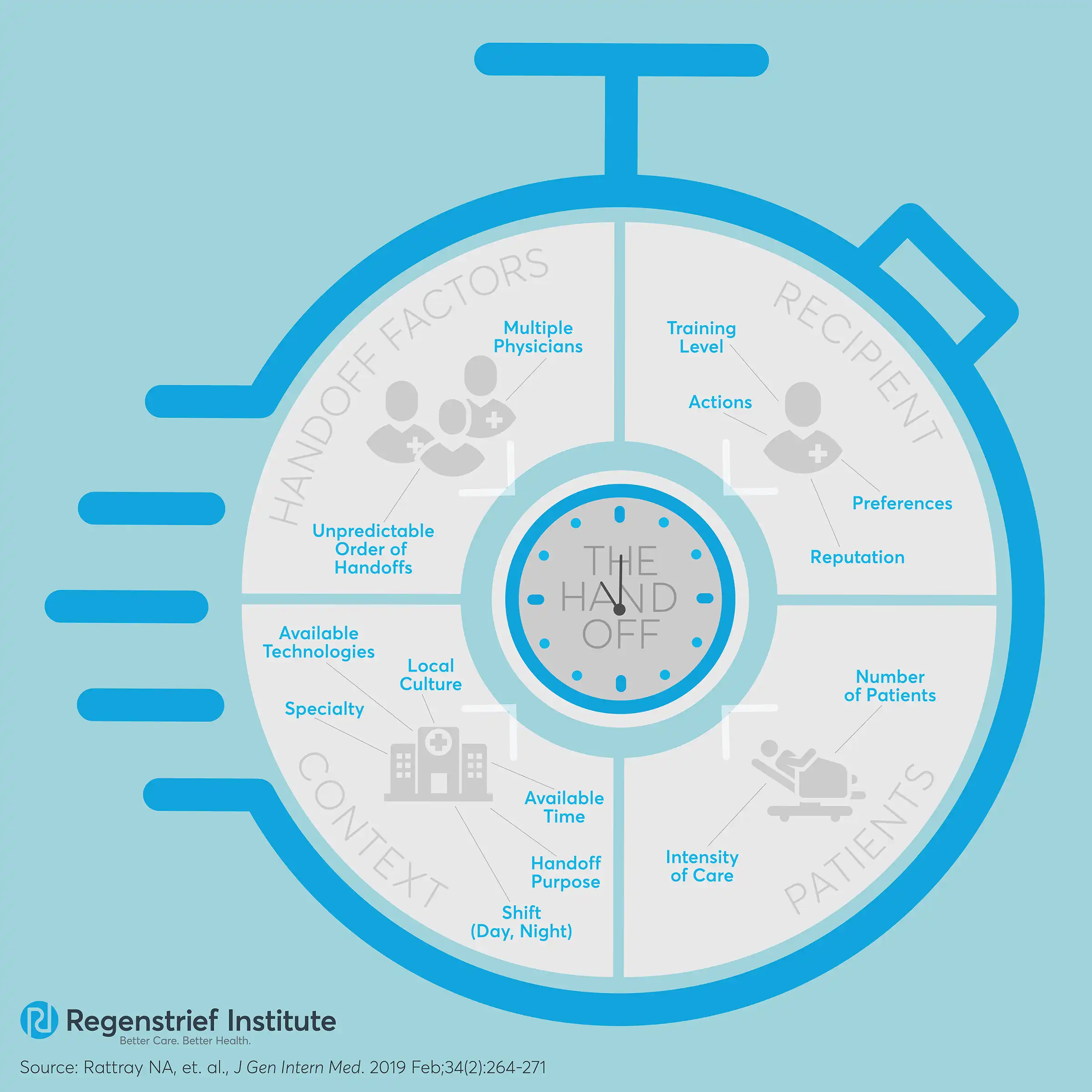
End-of-shift handoffs are complex interactions influenced by many factors, and changes need to be made to prepare medical residents to successfully execute the transitions. A team of research scientists highlighted the challenges and provided guidance on creating a systematic approach to teaching and carrying out transfers of care.
Researchers from Regenstrief Institute, the Department of Veterans Affairs, Indiana University School of Nursing, Wayne State University School of Medicine and Applied Decision Science, LLC interviewed medical residents from three VA medical centers across the country to learn more about handoffs. They published three papers from their findings.
End-of-shift handoffs pose a substantial patient safety risk. The transition of care from one doctor to another has been associated with delays in diagnosis and treatment, duplication of tests or treatment and patient discomfort, inappropriate care, medication errors and longer hospital stays with more laboratory testing. Handoff education varies widely in medical schools and residency training programs. There have been efforts to improve transfers of care, but they have not shown meaningful improvement.
“There is very little attention given to training for handoffs, but handoffs are very important for patient safety. Preparation, training and the way doctors and residents receive handoffs is very important,” said Regenstrief scientist Nicholas Rattray, Ph.D. “Attempts to design effective handoff interventions should balance the urge to standardize with the role of self and situation awareness.” Dr. Rattray, also a research health scientist for the VA, was the first author on two of the papers and a co-author on the other.
Researchers conducted interviews with 35 internal medicine and surgery residents at three VA medical centers about a recent handoff and analyzed the responses. The team also video-recorded and analyzed more than 150 handoffs.
In one paper, led by Laura Militello and published in The Joint Commission Journal of Quality and Patient Safety®, researchers detailed the importance of cognitive preparation for the handoffs. They identified six cognitive tasks residents engaged in before the handoff. These activities point to strategies for support via improved technology, organizational interventions and enhanced training. Those include a handoff tool that automatically populates key fields, creating a dedicated preparation time free from distractions and scenario-based simulation training.
Another finding of the study—medical residents said they were only partially prepared for enacting handoffs as interns, and experience is actually what taught them the most. In the paper published in BMC Medical Education, study authors discussed how formal education is not enough to teach effective handoffs. They offered recommendations to improve education, including:
- Establishing collaborative learning meetings among medical students, interns and residents.
- Providing point-of-care education programs connecting best practices with patient safety and efficacy goals.
- Using stories to make handoff curricula salient for learners.
- Enacting actual handoffs.
The third paper, just published in the Journal of General Internal Medicine, explains how the person receiving the handoff can affect the interaction. Medical residents said they changed their delivery based on the doctor or resident who was taking over. Study authors concluded that interventions designed to improve patient handoffs should more explicitly account for the role of the handoff recipient and not overemphasize standardizing the procedure.
In addition to his position at Regenstrief, Dr. Rattray is a research health scientist in the VA Health Services Research & Development Center for Health Information and Communication, Roudebush VA Medical Center.
Richard Frankel, Ph.D., was a senior scientist on the papers. He is a research scientist at Regenstrief, a core investigator at the VA HSR&D Center for Health Information and Communication, Roudebush VA Medical Center and a professor at the Indiana University School of Medicine.
Also involved in the project were Patricia Ebright, RN, Ph.D., from the Indiana University School of Nursing; Mindy E. Flanagan, Ph.D., and Zamal Franks from the HSR&D Center for Health Information and Communication, Roudebush VAMC; Laura G. Militello, M.A., from Applied Decision Science, LLC; Paul Barach, M.D., from Wayne State University School of Medicine; Shakaib U. Rehman, M.D., from Phoenix VA Health Systems and the University of Arizona College of Medicine-Phoenix; and Howard S. Gordon, M.D., from Jesse VAMC, VA HSR&D Center of Innovation for Complex Chronic Healthcare and the University of Illinois at Chicago.
“’Workin’ on Our Night Moves’: How Residents Prepare for Shift Handoffs” was published in The Joint Commission Journal on Quality and Patient Safety® in August 2018. Militello was the lead author on this paper.
“Content counts, but context makes the difference in developing expertise: a qualitative study of how residents learn end of shift handoffs” was published in BMC Medical Education in November 2018.
“‘Do You Know What I know?’: How Communication Norms and Recipient Design Shape the Content and Effectiveness of Patient Handoffs” was published in the Journal of General Internal Medicine in February 2019.
The research was funded by the Center for Health Information and Communication, Department of Veterans Affairs (VA), Veterans Health Administration, Health Services Research and Development Service (CIN 13-416), Project No. IIR 12 -090.