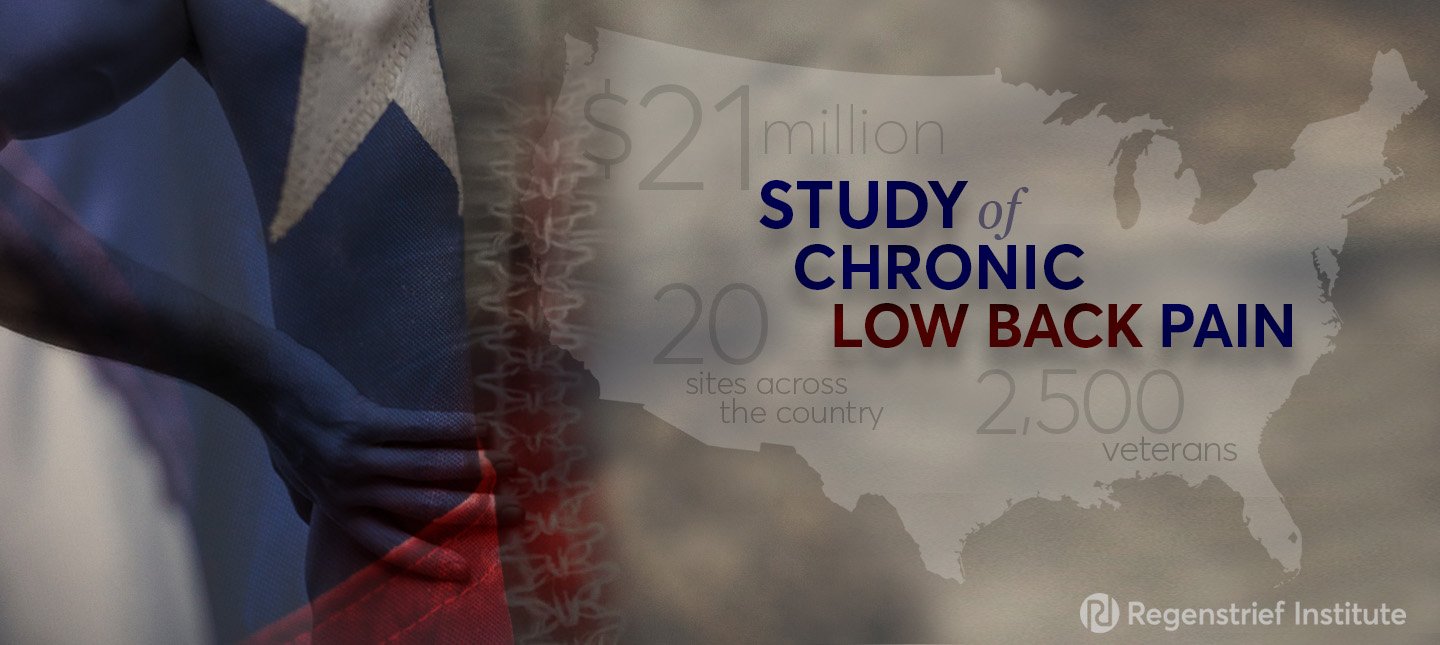
Matthew J. Bair, M.D., M.S., a research scientist with the Regenstrief Institute and the U.S. Department of Veterans Affairs, will co-lead a $21 million national study to find the best approach to manage chronic low back pain. The VA is funding the 20-site trial.
Dr. Bair is leading the study along with David Clark, M.D., PhD, a pain management physician at the VA Palo Alto Health Care System and Stanford University.
Low back pain is the most disabling chronic condition in the world. According to the National Institute of Neurological Disorders and Stroke, 80 percent of adults experience low back pain at some point in their lives. About 20 percent of people affected by acute low back pain develop chronic low back pain, which is defined as pain that lasts 12 weeks or more. Treating the condition is very challenging.
“We have an amazing opportunity to hopefully make a very large impact with this trial,” Dr. Bair said. “We believe this study could have greater implications for the treatment of chronic lower back pain in the general population.”
The study, called the Sequential and Comparative Evaluation of Pain Treatment Effectiveness Response (SCEPTER) trial, is a two-step sequential randomized pragmatic clinical trial. Unlike explanatory trials, pragmatic trials are designed to test the effectiveness of the intervention in a broad routine clinical practice. The first step of the trial will randomly divide participants among three different treatments. Some patients will be assigned to a web-based pain self-management program. Others will receive “enhanced physical therapy,” which will include some of the strategies from the web-based intervention combined with a physical therapist-directed exercise program that includes face-to-face appointments. The third group will receive usual care.
Step two will compare cognitive behavioral therapy, chiropractic care and a yoga-based intervention. Participants will be given the option to be randomized again, and if they prefer not to do one of those therapies, they will be allowed to opt out of that group and be randomized to one of the other two groups.
“This study is unique because it incorporates patient preferences,” said Dr. Bair, a research scientist with Regenstrief Institute and a core investigator with the VA Health Services Research and Development Center for Health Information and Communication at the Richard L. Roudebush VA Medical Center. “We feel that patient preferences do predict treatment response, so patients are more likely to benefit from a treatment they prefer than one they don’t.” Dr. Bair also is an associate professor of medicine at Indiana University School of Medicine.
The researchers are in the process of identifying the 20 sites for the trial. They hope to recruit more than 2,500 veterans to participate. The trial will last for six years.
“Chronic low back pain is very prevalent and can be debilitating,” said Dr. Clark. “All the interventions in this trial are evidence-based, and they have not been compared head-to-head. Because it is framed as a pragmatic trial, the hope is the findings can influence real-world clinical practice.”
The study also involves health economists, who will look at the costs of the interventions and the downstream consequences from an economic perspective.
The trial is funded through the VA Cooperative Studies Program.
In addition to Dr. Bair and Dr. Clark, who are co-principal investigators, other SCEPTER trial team members are Karleen Giannitrapani, PhD; Daniel Riddle, PhD; Erik Groessl, PhD; Jennifer Murphy, PhD; Diana Higgins, PhD; Paul Daughtery, D.C.; Ilana Belitskaya-Levy, PhD; and Mei-Chiung Shih, PhD.