New CDC study provides strong evidence that vaccines successfully combat severe disease
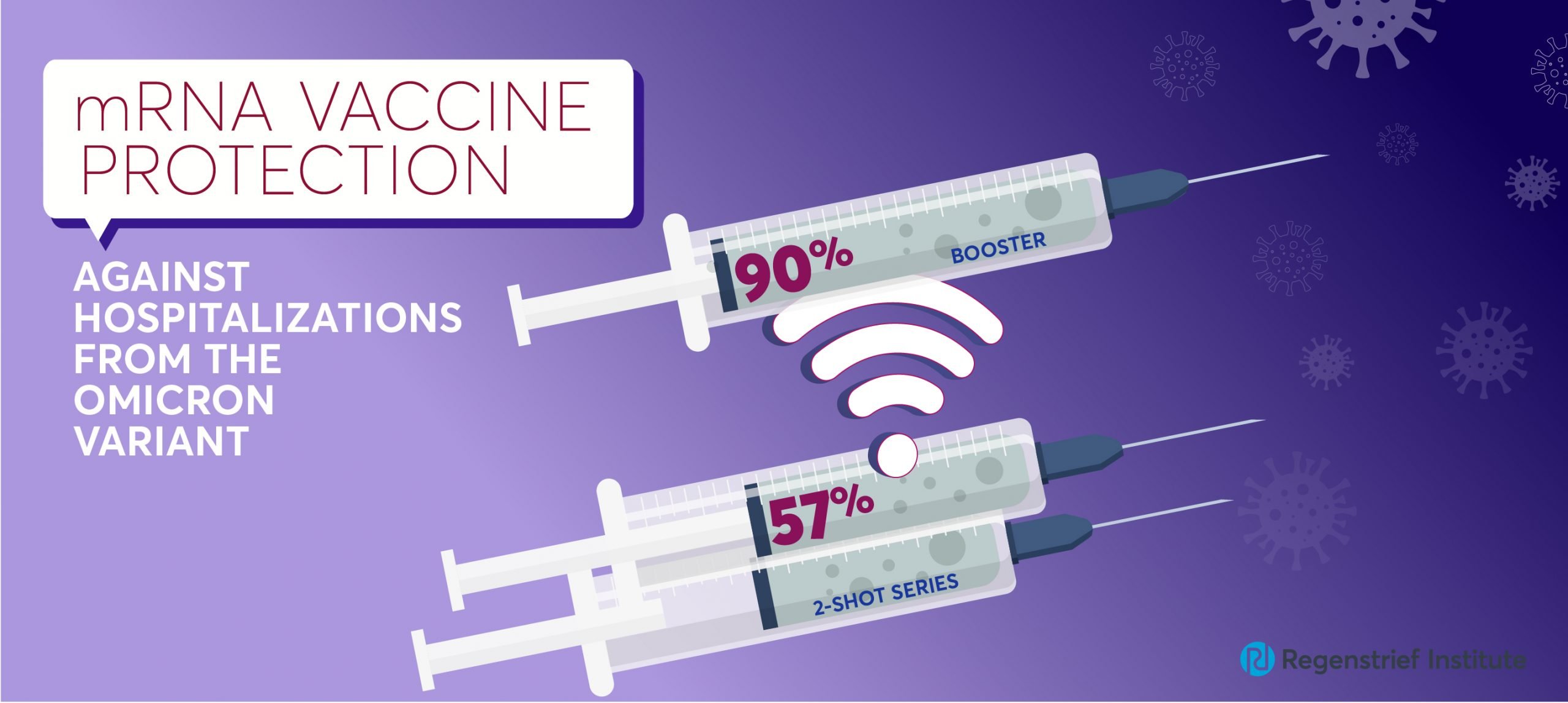
A nationwide study from the Centers for Disease Control and Prevention (CDC) has found that mRNA booster shots (either Pfizer or Moderna) are 82 percent effective in protecting against COVID-19 Omicron variant-associated emergency department (ED) visits and 90 percent effective in protecting against COVID-19 Omicron variant-related hospitalizations.
The value of the third dose of an mRNA vaccine is significant as two doses were only 38 percent effective in protecting against Omicron-related ED visits and only 57 percent effective in protecting against COVID-19 Omicron variant-related hospitalizations.
Boosters were even more effective against the Delta variant of COVID-19, protecting against 94 percent of both COVID-19 Delta variant-associated ED visits and hospitalizations.
“Our findings provide important evidence that booster shots are highly effective and those who are unvaccinated are at significantly greater risk of experiencing more severe COVID-19 outcomes and should get vaccinated and boostered as soon as possible,” said study co-author Shaun Grannis, M.D., M.S., vice president for data and analytics at Regenstrief Institute and professor of family medicine at Indiana University School of Medicine. “As we look at the high positivity rates across the nation, there is a silver lining. We have yet more evidence that vaccines and boosters offer protection against severe disease, including Omicron-related illness.”
“Effectiveness of a Third Dose of mRNA Vaccines Against COVID-19–Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance — VISION Network, 10 States, August 2021–January 2022” is published in the CDC’s Morbidity and Mortality Weekly Report.
The U.S. Centers for Disease Control and Prevention (CDC) collaborated with six U.S. healthcare systems plus the Regenstrief Institute, to create the VISION network to assess COVID-19 vaccine effectiveness. In addition to Regenstrief Institute, other members are Columbia University Irving Medical Center, HealthPartners, Intermountain Healthcare, Kaiser Permanente Northern California, Kaiser Permanente Northwest and University of Colorado. Regenstrief contributes data and expertise to the VISION Network.
Authors of the study are from 10 states and 14 institutions, including the public sector, research, clinical and academia. Regenstrief Institute authors, in addition to Dr. Grannis, are Brian E. Dixon, PhD, MPA, Regenstrief and IU Richard M. Fairbanks School of Public Health; William F. Fadel, PhD, a Regenstrief fellow; Nimish Ramesh Valvi, DrPH, MBBS, a Regenstrief fellow and Peter J. Embi, M.D., M.S., former Regenstrief president and a current affiliate scientist.
The other authors on the paper are Mark G. Thompson, PhD, CDC COVID-19 Response Team; Karthik Natarajan, PhD, Columbia University Irving Medical Center and New York Presbyterian Hospital; Stephanie A. Irving, MHS, Kaiser Permanente Northwest; Elizabeth A. Rowley, DrPH, Westat; Eric P. Griggs, MPH, CDC COVID-19 Response Team; Manjusha Gaglani, MBBS, Baylor Scott & White Health and Texas A&M University; Nicola P. Klein, M.D., Kaiser Permanente Vaccine Northern California; Malini B. DeSilva, M.D., HealthPartners Institute; Edward Stenehjem, M.D., Intermountain Healthcare; Sarah E. Reese, PhD, Westat; Monica Dickerson, CDC COVID-19 Response Team; Allison L. Naleway, PhD, Kaiser Permanente Northwest; Jungmi Han, Columbia University Irving Medical Center; Deepika Konatham, Baylor Schott & White Health; Charlene McEvoy, M.D., HealthPartners Institute; Suchitra Rao, MBBS, University of Colorado; Kristin Dascomb, M.D. Intermountain Healthcare; Ned Lewis, MPH, Kaiser Permanente Northern California; Matthew E. Levy, PhD, Westat; Palak Patel, MBBS, CDC COVID-19 Response Team; I-Chia Liao, MPH, Baylor Scott & White Health; Anupam B. Kharbanda, M.D., Children’s Minnesota; Michelle A. Barron, M.D., University of Colorado; Nancy Grisel, MPP, Intermountain Healthcare; Kristin Goddard, MPH, Kaiser Permanente Northern California; Duck-Hye Yang, PhD, Westat; Mehiret H. Wondimu, MPH, CDC COVID-19 Response Team; Kempapura Murthy, MPH, Baylor Scott & White Health; Julie Arndorfer, MPH, Intermountain Healthcare; Bruce Fireman, M.A. Kaiser Permanente Northern California,; Margaret M. Dunne, MSc, Westat; Eduardo Azziz-Baumgartner, M.D., CDC COVID-19 Response Team; Ousseny Zerbo, PhD, Kaiser Permanente Northern California; Catherine H. Bozio, PhD, CDC COVID-19 Response Team; Sue Reynolds, PhD, CDC COVID-19 Response Team; Jill Ferdinands, PhD, CDC COVID-19 Response Team; Jeremiah Williams, MPH, CDC COVID-19 Response Team; Ruth Link-Gelles, PhD, CDC COVID-19 Response Team1; Stephanie J. Schrag, DPhil, CDC COVID-19 Response Team; Jennifer R. Verani, M.D. CDC COVID-19 Response Team; Sarah Ball, ScD, Kaiser Permanente Northwest; Toan C. Ong, PhD, University of Colorado.
About Shaun Grannis, M.D., M.S.
In addition to his role as the vice president of data and analytics at Regenstrief Institute, Shaun Grannis, M.D., M.S., is the Regenstrief Chair in Medical Informatics and a professor of family medicine at Indiana University School of Medicine.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.