The gap remains unaltered despite changing attitudes toward mental health
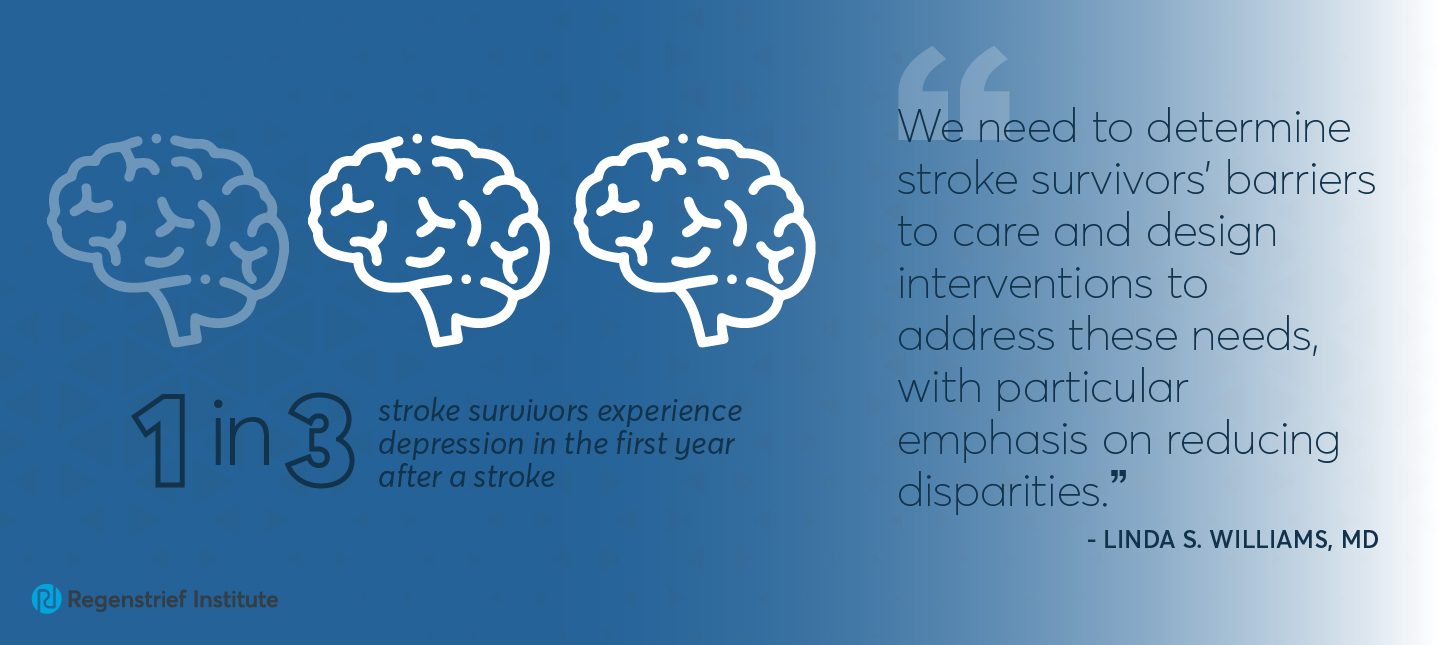
About one in three stroke survivors will experience depression in the first year after a stroke. A new study from Regenstrief Institute, Indiana University School of Medicine and University of Michigan shows two-thirds of those who screened positive for depression received no mental health treatment.
“This study shows a very significant number of survivors are not getting the help and support they need after a stroke,” said author Linda S. Williams, M.D., Regenstrief research scientist and IU School of Medicine professor of neurology. “This rate has remained low over more than a decade, despite societal changes in attitudes toward mental health treatment.”
The study analyzed data from a nationally representative sample of stroke and non-stroke patients from 2004 to 2017. The results showed that stroke patients used outpatient mental health services at a steady rate, however, the non-stroke population experienced an increase in depression treatment.
The study also revealed disparities in treatment. Older patients, men, and survivors who are Black or Hispanic were even less likely to receive treatment, and that trend remained the same throughout the duration of the study.
“Unmet needs for depression after stroke remain significant and are important because they impact stroke survivors’ quality of life and their recovery. Critical treatment gaps for vulnerable populations persist, and potential quality of care gaps may have widened between stroke and non-stroke patients,” said Dr. Williams. “We need to determine stroke survivors’ barriers to care and design interventions to address these needs, with particular emphasis on reducing disparities.”
“Trends in outpatient treatment for depression in survivors of stroke in the United States: 2004-2017” provides the first population-based data on temporal trends in outpatient treatment for depression among U.S. adults with stroke and calls for actions to improve care. It is published in Neurology®.
In addition to Dr. Williams, other authors are Liming Dong, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, and University of Michigan School of Public Health; and Briana Mezuk and Lynda D. Lisabeth, both of the University of Michigan School of Public Health.
About Linda S. Williams, M.D.
In addition to her role as a research scientist at Regenstrief, Linda S. Williams, M.D., is a core investigator for the U.S. Department of Veterans Affairs Health Services Research and Development Center for Health Information and Communication, Richard L. Roudebush VA Medical Center. She also is a professor of neurology at Indiana University School of Medicine
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.