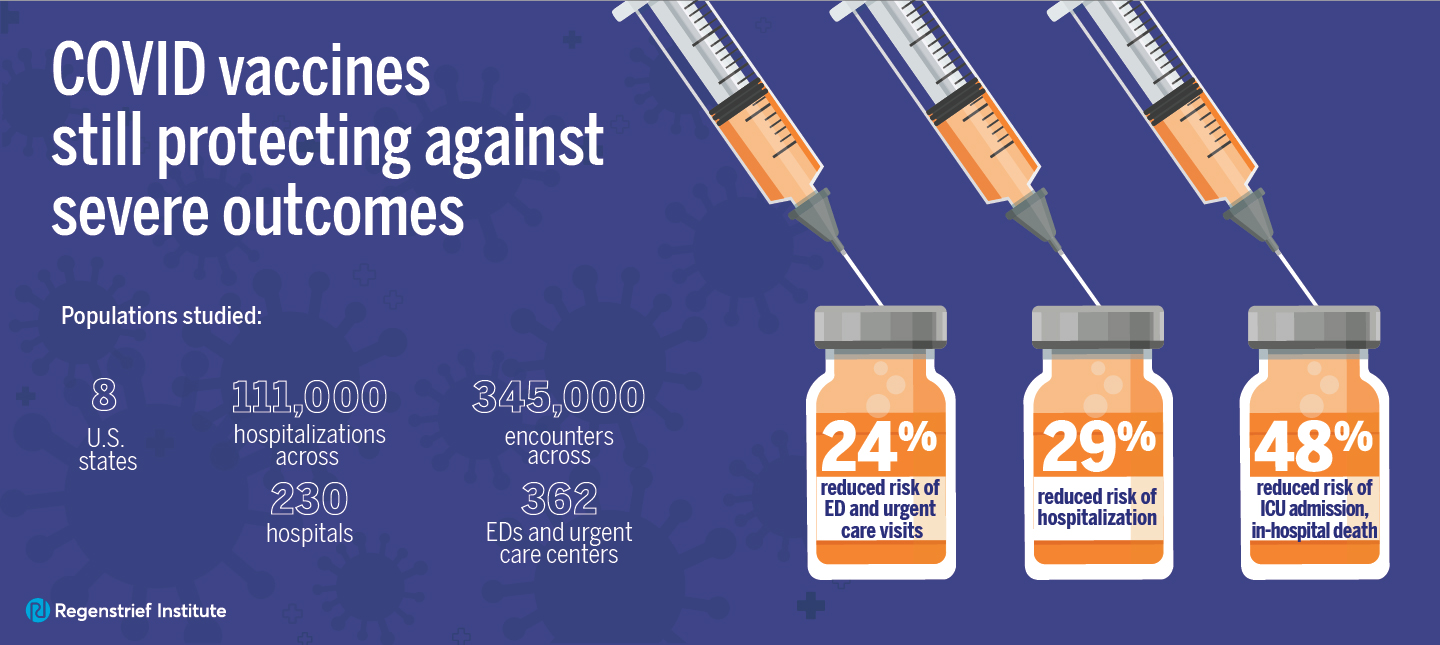
10-state June 2021-March 2023 study from CDC’s VISION Network identifies risk factors for critical outcomes
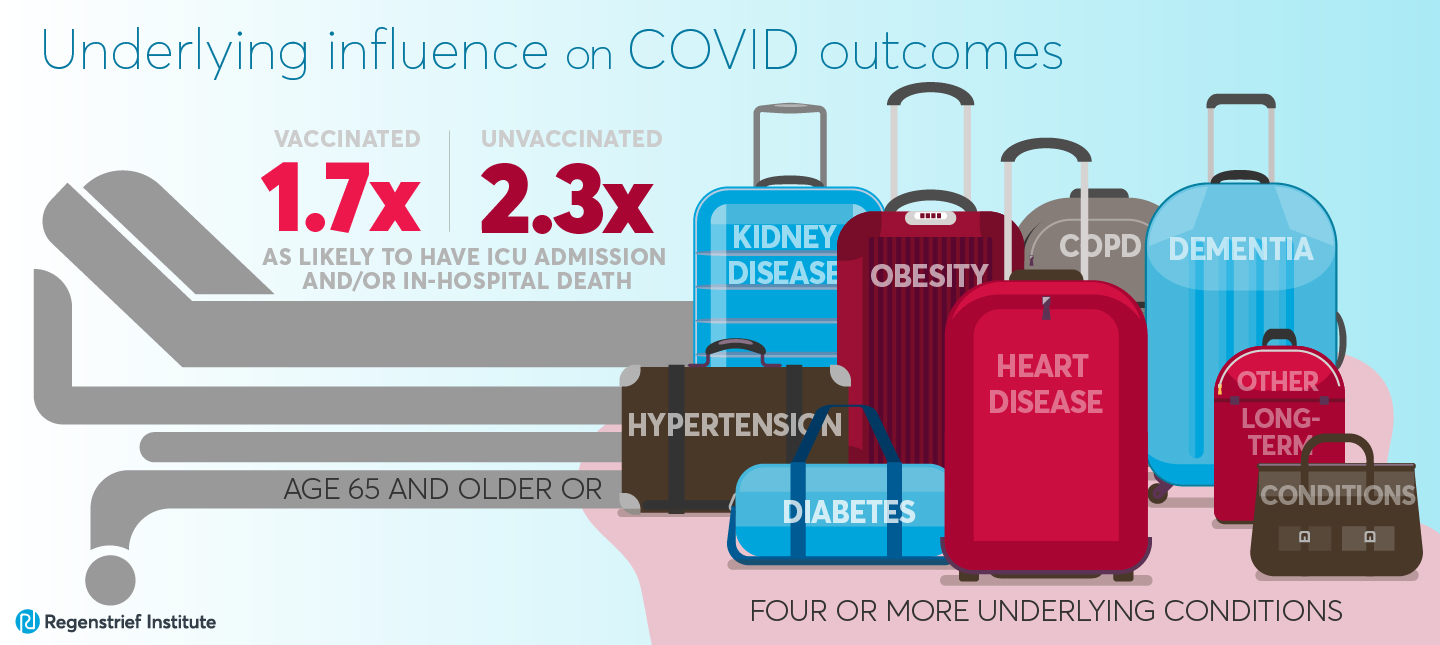
Whether vaccinated or not, having at least four disease risk factors put adults hospitalized due to COVID-19 at higher risk for critical outcomes, according to a 10-state study from the Centers for Disease Control and Prevention’s (CDC’s) VISION Network. The study describes the characteristics of adults hospitalized with COVID-19 from June 2021 through March 2023 and enumerates their risk factors for critical outcomes, defined as intensive care unit (ICU) admission and/or in-hospital death.
It is not uncommon for older adults hospitalized for COVID-19 to have four or more of these disease risk factors. The study authors note that this suggests that overall frailty may play a large role in susceptibility to critical disease regardless of vaccine status.
The majority of hospitalizations which resulted in ICU admission or death, regardless of vaccination status, were among male or female patients with multiple disease risk factors across multiple organ systems. Disease risk factors include hypertension, all types of diabetes, heart disease, chronic obstructive pulmonary disease (COPD), kidney disease, obesity, dementia and other long-term conditions.
Data from statewide immunization information systems, electronic health records and insurance claims of 60,488 individuals aged 18 or older from 10 states, who were hospitalized with COVID-19 across periods of Delta predominance to the post-BA.4/BA.5 period were analyzed.
From summer 2021 to spring 2023, the epidemiology of COVID-19 changed markedly. The researchers determined that the proportion of adults hospitalized with COVID-19 who experienced critical outcomes decreased with time, as did their hospital lengths of stay. Over the same time period the median patient age increased from 60 to 75 years.
“This is one of the first studies to examine and describe how the characteristics of seriously ill COVID-19 patients and the risk factors associated with those hospitalizations changed over time,” said study co-author Shaun Grannis, M.D., M.S., Regenstrief Institute vice president for data and analytics and a professor at Indiana University School of Medicine. “Our findings provide insight into factors that influence outcomes for hospitalized patients and can help us be alerted to those potential risks, so we can pay special attention to the most at-risk individuals.”
Vaccinated individuals, age 65 or older or with four or more underlying chronic medical conditions, were 1.7 times as likely to have a critical outcome. Unvaccinated individuals, age 65 or older or with four or more underlying medical conditions, were 2.3 times as likely to have a critical outcome. Both tendencies are in comparison to younger individuals or those with fewer than four disease risk factors.
“The number of patients hospitalized due to COVID-19 infection has decreased over time for a variety of reasons, including vaccination and natural immunity acquired due to past infection, advances in medical care as well as the severity of variants. But the virus hasn’t gone away and it’s important to note that people are still being infected or reinfected and are being hospitalized,” said study co-author Brian Dixon, PhD, MPA, interim director of the Center for Biomedical Informatics at Regenstrief Institute and professor at Indiana University Richard M. Fairbanks School of Public Health. “Our analysis shows that the people hospitalized for COVID who are at higher risk of an ICU stay or even an in-hospital death tend to be older and sicker with underlying conditions, some of which may be undiagnosed. If you are or have family members who are at higher risk, you and your family members should stay up to date on vaccinations and avoid spreading the disease with vulnerable members.”
“Clinical epidemiology and risk factors for critical outcomes among vaccinated and unvaccinated adults hospitalized with COVID-19 — VISION Network, 10 States, June 2021-March 2023” is published in Clinical Infectious Diseases, an official journal of the Infectious Diseases Society of America.
In addition to Drs. Grannis and Dixon, Regenstrief authors of this VISION Network study are Nimish R. Valvi, DrPH; Katie S. Allen, B.S.; William F. Fadel, PhD and former Regenstrief president and current affiliate scientist Peter Embi, M.D.
Complete author and affiliations list:
Eric P. Griggs, MPH1, Patrick K. Mitchell, ScD2, Victoria Lazariu, PhD2, Manjusha Gaglani, MBBS, FIDSA, FPID, FAAP3,4, Charlene McEvoy, M.D., MPH5, Nicola P. Klein, M.D., PhD6, Nimish R. Valvi, DrPH7, Stephanie A. Irving, MHS8, Noah Kojima, M.D.9, Edward Stenehjem, M.D., MSc10, Bradley Crane, M.S.8, Suchitra Rao, MBBS, MSCS11, Shaun J. Grannis, M.D., M.S.7,12, Peter J. Embi, M.D., M.S.13, Anupam B. Kharbanda, M.D.14, Toan C. Ong, PhD11, Karthik Natarajan, PhD15,16, Kristin Dascomb, M.D., PhD17, Allison L. Naleway, PhD8, Elizabeth Bassett, MPH2, Malini B. DeSilva, M.D., MPH5, Monica Dickerson, B.S.9, Deepika Konatham, B.S.18, Bruce Fireman, M.A.6, Katie S. Allen, B.S.7,19, Michelle A. Barron, M.D.11, Maura Beaton, M.S.15 Julie Arndorfer, MPH17, Gabriela Vazquez-Benitez, PhD5, Shikha Garg, M.D.9, Kempapura Murthy, MBBS, MPH18, Kristin Goddard, MPH6, Brian E. Dixon, PhD, MPA7,19, Jungmi Han, B.S.15, Nancy Grisel, MPP17, Chandni Raiyani, BDS, MPH18, Ned Lewis, MPH6, William F. Fadel, PhD7,19, Melissa S. Stockwell, M.D., MPH16,20,21, Mufaddal Mamawala, MBBS, MPH18, John Hansen, MPH6, Ousseny Zerbo, PhD6, Palak Patel, MBBS, MPH9, Ruth Link-Gelles, PhD, MPH1, Katherine Adams, MPH9 and Mark W. Tenforde, M.D.,PhD9.
1Coronavirus and Other Respiratory Viruses Division, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA; 2Westat, Rockville, Maryland, USA; 3Section of Pediatric Infectious Diseases, Department of Pediatrics, Baylor Scott & White Health, Temple, Texas, USA; 4Department of Medical Education, Texas A&M University College of Medicine, Temple, Texas, USA; 5Health Partners Institute, Minneapolis, Minnesota, USA; 6Kaiser Permanente Vaccine Study Center, Kaiser Permanente Northern California Division of Research, Oakland, California, USA; 7Center for Biomedical Informatics, Regenstrief Institute, Indianapolis, Indiana, USA; 8Kaiser Permanente Center for Health Research, Portland, Oregon, USA; 9Influenza Division, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention, Atlanta, Georgia, USA; 10Division of Infectious Diseases and Clinical Epidemiology, Intermountain Healthcare, Salt Lake City, Utah, USA; 11School of Medicine, University of Colorado Anschutz Medical Campus, Aurora, Colorado, USA; 12School of Medicine, Indiana University, Indianapolis, Indiana, USA; 13Vanderbilt University Medical Center, Nashville, Tennessee, USA; 14Children’s Minnesota, Minneapolis, Minnesota, USA; 15Department of Biomedical Informatics, Columbia University Irving Medical Center, New York, New York, USA; 16NewYork-Presbyterian Hospital ,New York, USA; 17Division of Infectious Diseases and Clinical Epidemiology, IntermountainHealthcare, Salt Lake City, Utah, USA; 18Department of Research Analytics and Development, Baylor Scott & White Research Institute, Baylor Scott & White Health, Temple, Texas, USA; 19Fairbanks School of Public Health, Indiana University, Indianapolis, USA; 20Division of Child and Adolescent Health, Department of Pediatrics, Columbia University Vagelos College of Physicians and Surgeons, New York, New York, USA; 21Department of Population and Family Health, Columbia University Mailman School of Public Health, New York, New York, USA.
About Shaun Grannis, M.D., M.S.
In addition to his role as the vice president for data and analytics at Regenstrief Institute, Shaun Grannis, M.D., M.S., occupies the Regenstrief Chair in Medical Informatics and is a professor of family medicine at Indiana University School of Medicine.
About Brian E. Dixon, PhD, MPA
In addition to his roles as interim director of the Regenstrief Institute’s Clem McDonald Center for Biomedical Informatics and director of public health informatics for Regenstrief Institute and Indiana University Richard M. Fairbanks School of Public Health, Brian E. Dixon, PhD, MPA, is a professor of epidemiology at the Fairbanks School of Public Health. He is also an affiliate scientist at the U.S. Department of Veterans Affairs Health Services Research and Development Center for Health Information and Communication, Richard L. Roudebush VA Medical Center.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform clinical practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.
About the Richard M. Fairbanks School of Public Health
Located on the IUPUI and Fort Wayne campuses, the Richard M. Fairbanks School of Public Health is committed to advancing the public’s health and well-being through education, innovation and leadership. The Fairbanks School of Public Health is known for its expertise in biostatistics, epidemiology, cancer research, community health, global health, health policy and health services administration.