There are political, legal and organizational barriers to overcome but sharing data with public health could improve chronic disease outcomes
As hospitalizations due to chronic conditions increase across the United States, attention is focusing on using data collected in electronic health records (EHRs) by healthcare systems to enable public health departments to gain understanding of the incidence and prevalence of hypertension, diabetes, asthma, obesity and other chronic diseases with the ultimate goal of improving disease outcomes.
In the U.S., 90 percent of clinicians, medical laboratories, imaging centers and other providers use EHR systems, providing ample data on individuals with access to healthcare. However, access to EHR data by public health departments is limited. Facilitating data sharing with public health departments is complex and requires health data aggregators such as health information exchanges as well as trust among data generators and data users.
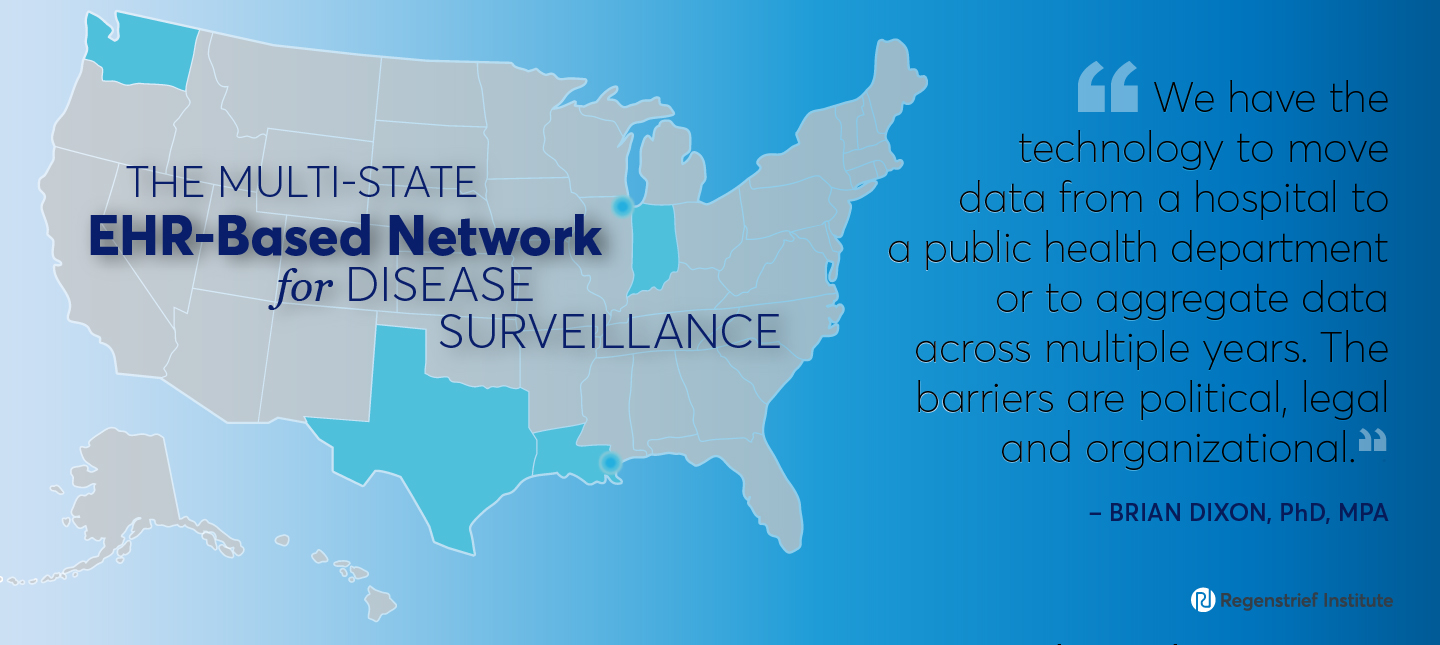
A research team including two Regenstrief Institute researchers presents practical guidance for implementing governance for sharing EHR data for chronic disease surveillance based on the experience of the Multi-State EHR-Based Network for Disease Surveillance.
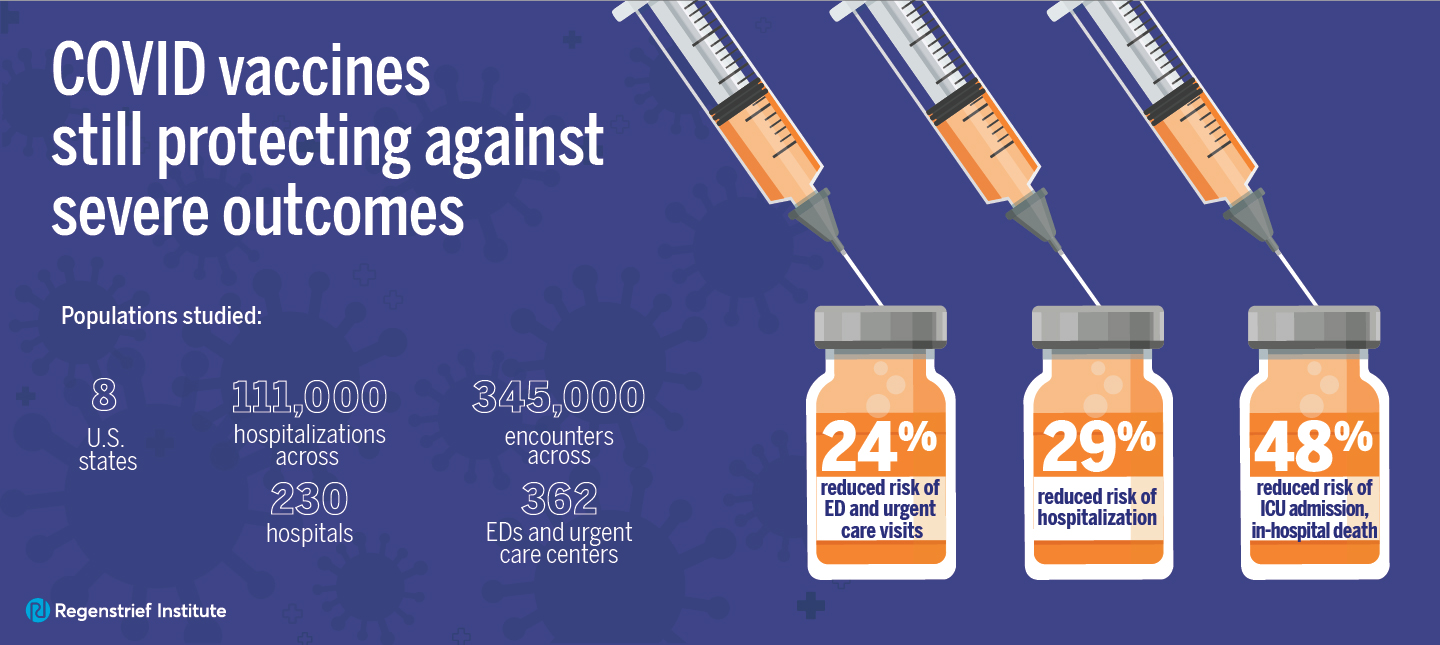
Harnessing the power of health information technology to track infectious diseases has provided vital, in-depth insight to public health departments into infections, hospitalizations, deaths, vaccinations and more during the COVID-19 pandemic.
Unlike infectious diseases, however, there are no legal requirements that chronic diseases be reported to public health departments. Yet if city, county and state public health departments could learn about individuals living with chronic conditions from EHR data via a health information exchange or other data sharing mechanism, they can make a difference in numerous ways according to the Regenstrief Institute’s Center for Biomedical Informatics Interim Director Brian Dixon, PhD, MPA, senior author of the paper.
“With data to identify populations, public health agencies could monitor specific geographic areas for increasing or decreasing numbers of cases of a particular disease and drive people living with chronic conditions to a better quality of life and better disease outcomes,” Dr. Dixon said. “For example, if one part of a city or state has an increasing rate of new cases of diabetes perhaps individuals aren’t getting the education and care they need. Or if in another section of a city or state there is a moderate amount of hypertension but bad outcomes, maybe they’re not taking their medications and need support. Public health department budgets are tight, but they can provide services targeted to chronic diseases.
“I think this paper is very important for policymakers and public health leaders because it specifically outlines the processes and policies that we need to enable this kind of work – which doesn’t happen overnight – to occur. Like many things in informatics, the technology exists to aggregate and analyze data on chronic disease. We have the technology to move data from hospital A to a public health department or to aggregate data across multiple years,” said Dr. Dixon. “The barriers are political, legal and organizational. And so, governance and policy are what you use to address and break down those barriers and work within legal parameters to share data. To sustain this activity, we will need to put this kind of governance and these kinds of policies in place to enable EHR-based chronic disease public health surveillance and intervention to occur everywhere in the U.S.”
The current gold standard for chronic disease surveillance is an annual random digit telephone health survey conducted by the U.S. Centers for Disease Control and state health departments. The survey provides reliable metrics about chronic disease on a small but representative sample of the population. However, it takes approximately two years for the data to be available. EHR-based public health surveillance would significantly reduce the delay. Additionally, data would be clinical rather than self-reported.
Dr. Dixon notes that chronic disease surveillance using EHR data requires trust between healthcare systems and public health departments. Building trust, he says, requires robust intentional governance policies and procedures as outlined in the paper.
The Multi-State EHR-Based Network for Disease Surveillance is composed of data contributors and health departments representing Texas, New Orleans, Louisiana, Chicago, Washington and Indiana. The paper reported that the network’s governance approach resulted in a transparent governance framework cultivating trust across the network.
“Fostering Governance and Information Partnerships for Chronic Disease Surveillance: The Multi-State EHR-Based Network for Disease Surveillance” is published in Journal of Public Health Management & Practice.
Regenstrief authors are Dr. Dixon and Shaun Grannis, M.D., M.S., the institute’s vice president for data and analytics.
All authors of the study:
Kraus, Emily McCormick, PhD, MPH; Saintus, Lina, MPH; Martinez, Amanda K., MPH, MSN, R.N.; Brand, Bill, MPH; Begley, Elin, MPH; Merritt, Robert K., M.A.; Hamilton, Andrew, M.S., BSN, R.N.; Rubin, Rick, B.A.; Sullivan, Amy, PhD, MPH; Karras, Bryant Thomas, M.D.; Grannis, Shaun, M.D., M.S.; Brooks, Ian M., PhD; Mui, Joyce Y., B.S., MPM; Carton, Thomas W., PhD, M.S.; Hohman, Katherine H., DrPH, MPH; Klompas, Michael, M.D., MPH; and Dixon, Brian E., PhD, MPA.
Author affiliations as listed in the publication:
The Task Force for Global Health, Public Health Informatics Institute, Decatur, Georgia (Dr Kraus, Ms Saintus, and Mr Brand); Kraushold Consulting, Denver, Colorado (Dr Kraus); National Association of Chronic Disease Directors, Decatur, Georgia (Ms Martinez and Dr Hohman); Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia (Ms Begley and Mr Merritt); AllianceChicago, Chicago, Illinois (Mr Hamilton); OneHealthPort, Seattle, Washington (Mr Rubin); Washington State Department of Health, Tumwater, Washington (Drs Sullivan and Karras); Center for Biomedical Informatics, Regenstrief Institute, Indianapolis, Indiana (Drs Grannis and Dixon); Indiana University School of Medicine, Indianapolis, Indiana (Dr Grannis); Health Data Compass, University of Colorado Anschutz, Aurora, Colorado (Dr Brooks and Ms Mui); Louisiana Public Health Institute, New Orleans, Louisiana (Dr Carton); Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston, Massachusetts (Dr Klompas); and Indiana University Fairbanks School of Public Health, Indianapolis, Indiana (Dr Dixon).
The “Improving Chronic Disease Surveillance and Management Through the Use of Electronic Health Records/Health Information Systems” project is supported by the Centers for Disease Control and Prevention (CDC).
About Brian E. Dixon, PhD, MPA
In addition to his role as the director of public health informatics at the Regenstrief Institute and Indiana University Richard M. Fairbanks School of Public Health at IUPUI, Brian E. Dixon, PhD, MPA, is the interim director and a research scientist with the Clem McDonald Center for Biomedical Informatics at Regenstrief Institute and an associate professor of epidemiology at the Indiana University Fairbanks School of Public Health at IUPUI. He is also an affiliate scientist at the U.S. Department of Veterans Affairs Health Services Research and Development Center for Health Information and Communication, Richard L. Roudebush VA Medical Center.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform clinical practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About the IU Richard M. Fairbanks School of Public Health
Located on the IUPUI and Fort Wayne campuses, the IU Richard M. Fairbanks School of Public Health is committed to advancing the public’s health and well-being through education, innovation, and leadership. The Fairbanks School of Public Health is known for its expertise in biostatistics, epidemiology, cancer research, community health, global health, health policy, and health services administration.