Benefits may not always outweigh the risks for this vulnerable population.
It is common for individuals seeking medical care for symptoms of concern to go to the nearest hospital. Physicians there may determine the facility cannot provide the care they believe the patient needs and recommend transfer to another hospital offering a higher level of care or specialized services.
In a recent study, researchers from Regenstrief Institute and Indiana University School of Medicine reviewed electronic health records to compare older adults with dementia transferred to another hospital with older adults who did not have dementia. The researchers found significant differences in treatment following transfer.
- Patients with dementia more often received a geriatrics or palliative care consultation after transfer.
- Patients with dementia were less likely to be full code (full resuscitation support) at admission after transfer.
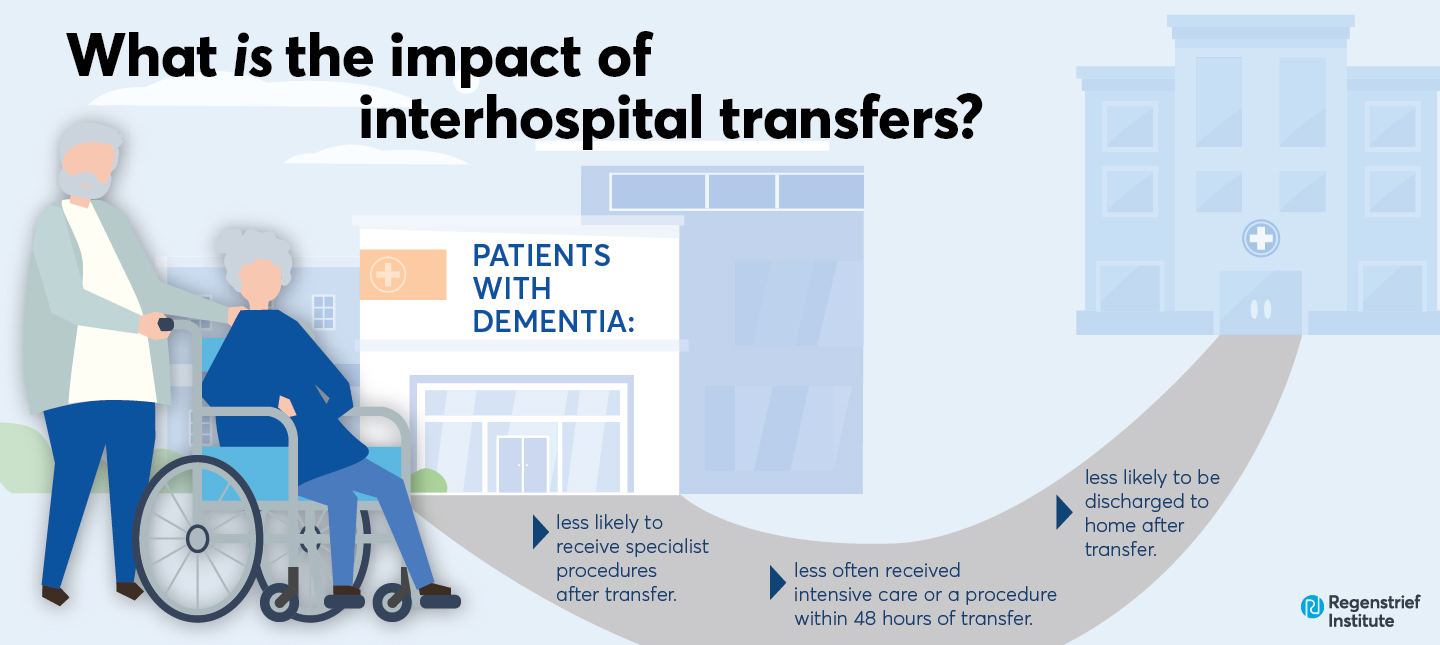
- Patients with dementia were less likely to be discharged to home after transfer.
- Patients with dementia less often received intensive care or a procedure within 48 hours of transfer.
- Patients with dementia were less likely to be admitted to an intensive care unit (ICU) after transfer.
- Patients with dementia were less likely to receive specialist procedures after transfer.
Dementia did not significantly influence the odds of death prior to discharge following interhospital transfer, however, older age, male gender, and “do not resuscitate” (DNR) code status were associated with higher odds of death.
“Our findings, which show that older adults with dementia were less likely to receive intensive care or a medical procedure within the first two days of transfer, highlight the need to focus very closely on the patient with dementia and their family to determine if transfer provides optimal care and to build out our infrastructure in a way that supports that,” said study senior author and geriatrician Malaz Boustani, M.D., MPH, of Regenstrief Institute and IU School of Medicine. “For example, telecare rather than transfer to a tertiary care center may be the answer for many patients in this vulnerable population.”
“When it comes to transfers, there are potentially significant risks to the patient population of older adults with dementia as well as other factors that we ought to be taking into account and discuss with the family and patient prior to transfer,” said study co-author and geriatrician Kathleen Unroe, M.D., MHA, of Regenstrief Institute and IU School of Medicine. “It might be hard for the 85-year-old spouse to drive an hour and a half to the next hospital to participate in discussions about the patient’s care. So, we are reassessing the question about whether these transfers make sense and are the best quality of care for people with dementia.”
“Transfer centers, which coordinate the patient transfer process, are now common in the United States. In next generation transfer centers, I’d like to see a care coordinator who can help facilitate expert, detailed evaluation of all options with the patients and their families in a way that leads to a truly comprehensive discussion of risks, benefits, and alternatives for this vulnerable group of patients,” said study first author and emergency medicine physician Nancy Glober, M.D. of IU School of Medicine. “We ought to be very considerate and focused on patient centered care, particularly in this population.”
“Impact of interhospital transfer on patients with Alzheimer’s disease and other related dementia” is published in Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring.”
Authors:
Nancy Glober1, Alexandra LaShell1, Nicholas Montelauro1, Lindsay Troyer1, Michael Supples2, Kathleen Unroe1,5, Christopher Tainter3, Greg Faris1, Mikita Fuchita4, and Malaz Boustani1,5
Affiliations
1 Indiana University School of Medicine Indianapolis Indiana USA.
2 Department of Emergency Medicine Wake Forest School of Medicine Winston-Salem North Carolina USA.
3 University of California at San Diego La Jolla California USA.
4 University of Colorado Hospital Aurora Colorado USA.
5 Regenstrief Institute, Indianapolis Indiana, USA
This work was supported by Grant 2021258 from the Doris Duke Charitable Foundation through the COVID-19 Fund to Retain Clinical Scientists collaborative grant program and was made possible through the support of Grant 62288 from the John Templeton Foundation.
About Malaz Boustani, M.D., MPH
In addition to his role as a research scientist at Regenstrief Institute, Malaz Boustani, M.D., MPH, is the founding director of the Center for Health Innovation and Implementation Science. He is the Richard M. Fairbanks Professor of Aging Research at Indiana University School of Medicine. Dr. Boustani is also director of care innovation at Eskenazi Health.
About Kathleen T. Unroe, M.D., MHA
In addition to being a research scientist at Regenstrief Institute, Kathleen Unroe, M.D., MHA, is an associate professor of medicine at Indiana University School of Medicine and a practicing geriatrician.
About Nancy Glober, M.D.
Nancy Glober, M.D., is an assistant professor of emergency medicine at Indiana University School of Medicine. She is also director for downtown hospitals of Indiana University Health Transfer Center.
About Regenstrief Institute
Founded in 1969 in Indianapolis, Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform clinical practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.