Study identifies three major areas to reduce burnout and increase work engagement
Clinician burnout in healthcare is a growing area of concern, especially as the COVID-19 pandemic stretches on. Research from the U.S. Department of Veterans Affairs and Regenstrief Institute looked at ways organizations can address burnout.
“There is plenty of attention on burnout these days, but the approaches we use to combat it are often centered around building coping skills for staff. But burnout isn’t something we can just train out of people. Resiliency and self-care workshops can be helpful to some people but are not enough,” said first author Angela Rollins, PhD, associate director of the VA Health Services Research and Development (HSR&D) Center for Health Information and Communication (CHIC) at Richard L. Roudebush VA Medical Center and research scientist at Regenstrief Institute. “Organizational level interventions need to be implemented to make sure job demands and resources are in balance, which should help prevent many cases of burnout.”
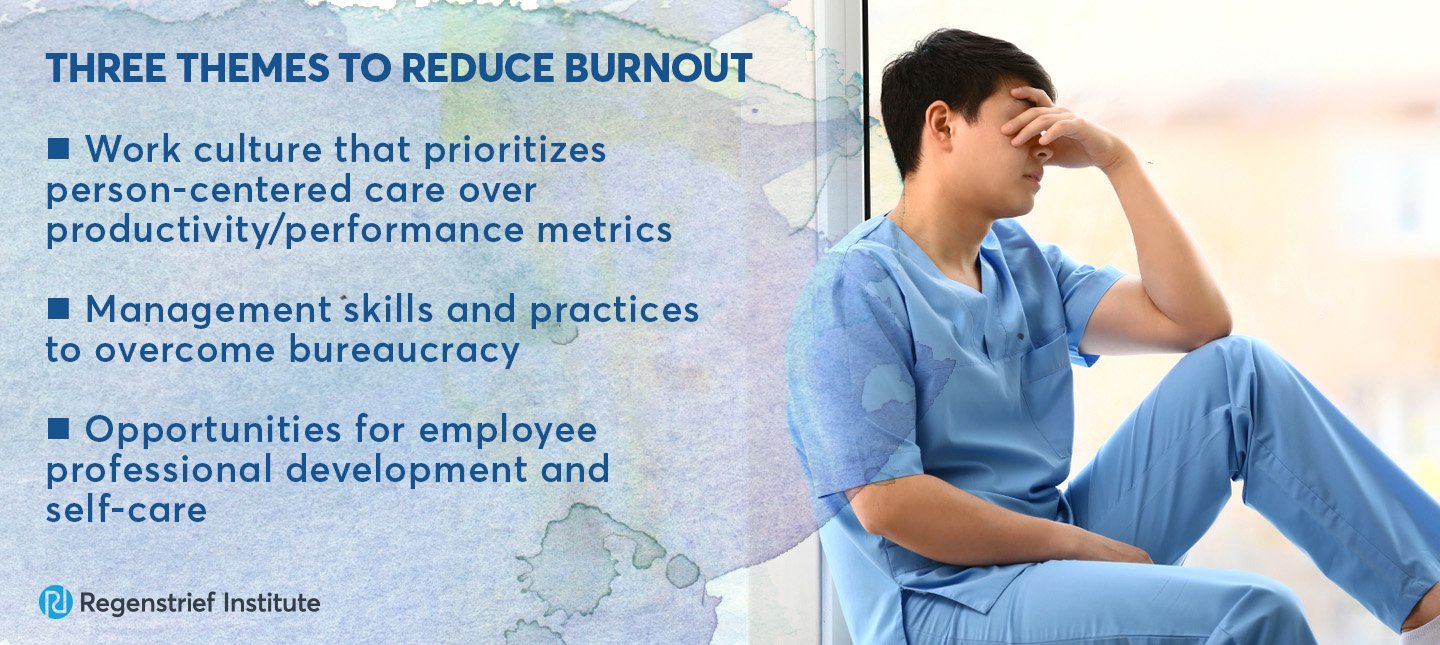
The research team interviewed 40 mental health clinicians and managers from a variety of healthcare systems who were participating in a burnout intervention. The team determined results of those interviews could be broken down into three themes around how organizations might reduce burnout.
- A work culture that prioritizes person-centered care over productivity and other performance metrics.
- Management skills and practices to overcome bureaucracy.
- Opportunities for employee professional development and self care.
“Clinicians told us that they chose this line of work because they wanted to help people. When policies get in the way of providing good care, it undermines morale and engagement,” said Dr. Rollins. “This particular study focused on mental health providers, but this is likely applicable to all healthcare professions. This isn’t an issue that can be solved at the individual or supervisor levels. The health system is out of balance, and that needs to be addressed. This research can be used to inform the development of health system, organizational and program-level initiatives.”
“Organizational conditions that influence work engagement and burnout: A qualitative study of mental health workers” is published in the Psychiatric Rehabilitation Journal. The paper is part of a special section that focuses on aspects of worker wellbeing and explores potential action steps.
Regenstrief research scientist and VA HRS&D CHIC core investigator Johanne Eliacin, PhD, is also an author on the paper. Other authors include Alissa L. Russ-Jara, PhD, of VA HSR&D CHIC; Maria Monroe-Devita, PhD, of University of Washington School of Medicine; Sally Wasmuth, PhD, of VA HSR&D CHIC; Mindy E. Flanagan, PhD, of VA HSR&D CHIC; Gary A. Morse, PhD of Places for People; Michael Leiter, PhD, of Acadia University; and Michelle P. Salyers, PhD, of the IUPUI ACT Center of Indiana.
This work was supported by VA Health Services Research and Development Service (HSR&D) IIR 11-030 (PI: Rollins). Drs. Rollins, Eliacin, and Russ were also supported in part by VA HSR&D Center for Health Information and Communication, CIN 13-416. Dr. Russ and Eliacin were supported in part by VA HSR&D Career Development Awards: CDA 11-214 (PI: Russ) and CDA 16-153 (PI: Eliacin).
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About the VA Health Services Research and Development Center for Health Information and Communication
The Health Services Research and Development (HSR&D) Center for Health Information and Communication (CHIC) group is a diverse cadre of researchers within Veterans Health Indiana joining together to transform the healthcare system, both within and outside the VA, so every patient receives consistent, high-quality care.
About Angela Rollins, PhD
In addition to her role as a research scientist at Regenstrief Institute, Angela Rollins, PhD, is a core investigator and associate director for the U.S. Department of Veterans Affairs Health Services Research and Development Center for Health Information and Communication, Richard L. Roudebush VA Medical Center. She also serves as the research director for the ACT Center of Indiana and an associate research professor of psychology at IUPUI.