How does the way we talk about pain affect our society? We’ve been told that certain drugs are the most effective ways to relieve pain, but is that true? Featuring interviews with Kurt Kroenke, MD, MACP and Marianne Matthias, PhD.
Transcript
Phil Lofton:
From the Regenstrief Institute, this is The Problem. The Problem is an anthological podcast dedicated to fighting the Hydra s of healthcare – those complicated, big, hairy issues that impact healthcare on the societal level. Every season you’ll hear about a different big, massive problem and each episode within that season will feature a different discipline or industries take on that problem, how it’s being addressed and what’s being talked about and the trials and triumphs of those involved clinically and personally. This season is all about opioids. Over this series of episodes The Problem willl talk about how we – local communities, Indiana and the United States – got into this crisis, how people suffering from addiction are treated and how the needle can be moved on addiction. This is a podcast for anyone who might be interested in how these problems have developed and how they’re approached. You don’t need a PhD to be affected by them, so you shouldn’t need a PhD to learn more about them. Regenstrief Institute is a global leader dedicated to improving health and healthcare through innovations and research and biomedical informatics, health services and aging. Welcome to The Problem.
[OW Sound Collage]: 01:12 [OW Sound Collage]
Phil Lofton: 01:27
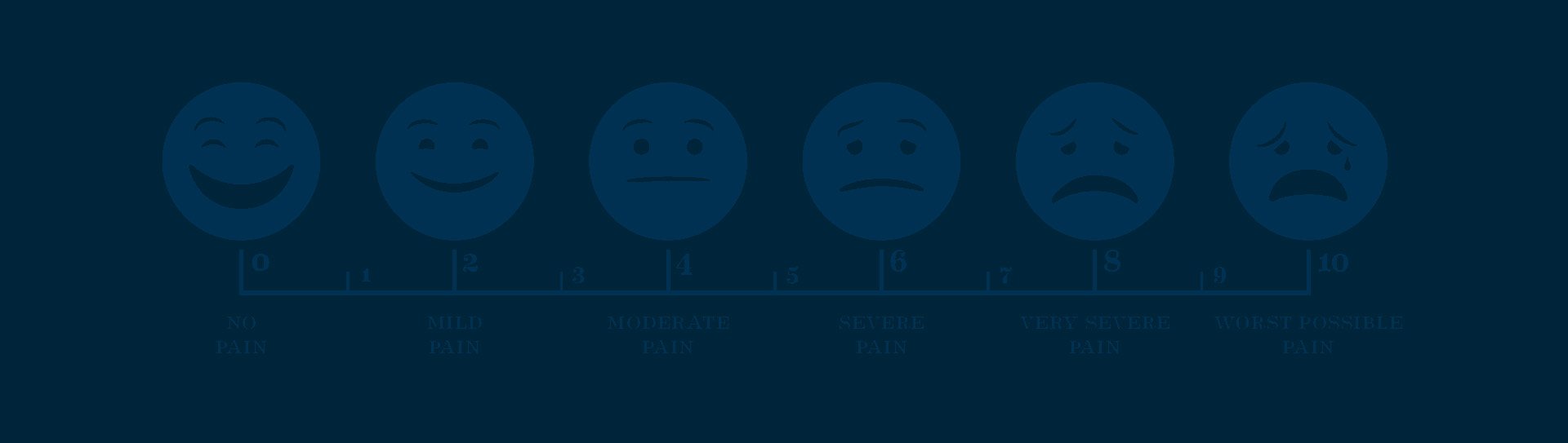
Ow! it’s one of the first words we learn as humans, but we learn the principle behind it even earlier. I’m in pain and I would like it to stop. We communicate it in the simplest, most elemental ways possible with an ow or a scream or a cry. Then we get older. As we grow into our bodies and begin to understand them better, we grow our capacity to communicate or pain with people who can help relieve it. I’ve got an Owie becomes, ‘Hey doc, my knee’s been hurting since I fell on it last week’ and that greater level of communication opens the door for more effective treatment. Health Communications is the study and practice of communicating health information that can mean broad public health campaigns, targeted promotions and communities. We’re exploring the ways that doctors and patients talk about health with each other. These are all pretty primal essential ideas that have been wrapped up in the practice of medicine since day one, but the field wasn’t officially recognized until the 1970’s when the International Communication Association acknowledged it.
Phil Lofton: 02:26
In the clinic, health communication is all about making sure that patients have the ability to accurately describe their symptoms to their doctors and that doctors have the ability to make their patients understand what treatments they’ll be receiving, how their diseases will affect them, and any associated side effects. On the public health level, health communication tries to get community members to understand things around them that might be affecting their health or behaviors that are spreading in the community that should be avoided. One of the big ways that health communication measures success Is through health literacy, understanding the necessary health free of jargon. This health literacy is measured a few different ways a researcher might have the patient take a short quiz before and after receiving a flyer or watching a video, in other instances, the researcher might have the patient describe the health information back to them.
Phil Lofton: 03:15
This is called a teach back. No matter how the information is collected, the standards for success are the same. If the patient has become better at understanding and communicating the health issue, then it’s a job well done.
Phil Lofton: 03:27
In this episode we’re talking to two scientists who are working hard to improve the ways we approach pain in the clinic. We’ll learn about the history of how we talk about pain, how it’s contributed to the opioid crisis, and how changing the way doctors talk to patients about pain and about medicine can lead to better lives. From the Regenstrief institute, this is The Problem. I’m your host, Phil Lofton.
Phil Lofton: 04:12
Kurt Kroenke is a legend. If you’ve ever been screened for depression, there’s a pretty big chance that your doctor used a tool called the PH-Q 9 that was developed by Dr Kroenke and his team,
Phil Lofton: 04:24
But it’s pretty likely that some of you, even those of you who have taken this screening tool, have never heard of it. So let’s unpack it real quick.
Phil Lofton: 04:33
The PH-Q 9 is a quick, simple nine question questionnaire that helps doctors monitor depression. Patients respond to questions about how often they’ve struggled with depressive symptoms like trouble sleeping or suicidal thoughts. At the end they tell their doctor how difficult the symptoms have made their life. Dr. Kroenke is a clinician, meaning he’s a doctor who sees patients on a regular basis in the clinic. He’s also had a long and successful career in research.
Kurt Kroenke: 04:58
I’d had a, the first half of my career, I was a physician in the army. I got in because they hit a program they paid for your medical school and uh, then I enjoyed what I was doing. So I stayed in about 20 years at four different teaching hospitals. And then for the last 21 years I’ve been at Indiana University, so it sort of divides itself in halves and a part of that time in Indiana University I sort of took care of veterans in the VA Clinic as well as patients outside the VA, in Eskenazi.
Phil Lofton: 05:31
Over the course of his career, he’s focused on symptoms, the way we measure them, the way we talk about them and the way we treat them.
Kurt Kroenke: 05:37
Yeah. So you’re correct. I got interested in symptoms by the way, because it’s about half of all the reasons people come in to see a physician, but a lot of times we focus on diseases and sometimes the symptoms as representative of disease and sometimes it’s what I call a “symptom-only diagnosis” like headache, fatigue, pain. I got into pain in particular the last decade or so, because, first pain accounts for half of all physical symptoms, headache, chest pain, musculoskeletal pain, back pain. So it’s the most common and there’s been a lot of emphasis, especially the last 20, 25 years on, on better treatment of pain. And more funding for pain. I’m a researcher, so it tended to be a more popular symptom.
Phil Lofton: 06:22
In the past few decades. Dr Kroenke has seen a large shift in the way we talk about pain.
Kurt Kroenke: 06:26
Say there’s been a couple waves. So when I first started out, pain was always felt to be an indicator of something else. Something specific. As I mentioned earlier, there’s this disease model. We think everything crosses back to a disease, but there’s a lot of pain that’s mainly a symptom somewhere in the body and we are testing doesn’t help us, you know, MRIs, blood tests and so forth. So then a little over 25 years ago, the early two thousands, there was a movement to represent, to recognize pain as an entity onto itself and a more humane approach to pain. So there was a big push to recognize pain, better treat pain, look at pain as any other disease because it causes a lot of suffering. So there was a big push to screen for pain, treat pain. And along with that came the issue of using more opiates.
Phil Lofton: 07:27
Now that’s true. In fact, Americans consume 99 percent of hydrocodone. The US also leads the rest of the world by a very comfy margin for total opioids prescribed. But why?
Kurt Kroenke: 07:38
Yeah, there’s different theories for that. One is we had this particular push advocacy movement, which was a good one to better treat chronic pain. And maybe the thing we didn’t understand so well is the downside of opioids. And also, we always call them strong painkillers, but when you compare them to other non-opiate pain medicines we have, they aren’t much that much stronger than we thought. So there was a certain that there is a certain mystery about the fact they were stronger than we thought. And uh, the downside was less than we thought. I think that’s second reason ends up being probably partly true, the conspiracy theory that the pharmaceutical companies that marketed the opiates were pushing him and there’s probably some truth that they were heavily marketed in the US. And so you had these two forces. One was pushing doctors to say you everything you can to treat chronic pain. And the thought was, here’s, here’s the strongest painkiller we have. And then there was probably a marketing push too. and the two together led to over prescribing.
Phil Lofton: 08:52
And even more interestingly, while we were being told that these pills were the best and most effective way to reduce pain, it turns out that’s not the case.
Kurt Kroenke: 09:00
So that trial, the SPACE trial, was published in Jama this year. The lead author is Erin Krebs, who used to be a fellow and faculty here, worked with us as part of our team and then moved to Minnesota, Minneapolis, the VA there, and planned a study here and she completed it there. And what she found out very simply as she took several hundred primary care patients, veterans with chronic pain and who his pain was such, it hadn’t been well treated by other treatments. And so, in an older world we might’ve started opiates and a randomized or allocated half the patients receiving opiates for a year and half of the patients receiving pain medicines that were not opiates. Okay. And the outcomes were equal. So both groups got improvement in pain and the improvement was not greater in the opiate group than those who didn’t get opiates.
Kurt Kroenke: 10:02
But the side effect rate was a little higher. Take home message, which people had already started to believe, this kind of really put the icing on the cake, was that we probably should be reluctant to start opiates and chronic pain, especially early because the mystery we had about opiates are stronger if you use the right combination of other pain treatments, you may in the average patient get nearly as good outcomes.
Phil Lofton: 10:32
Gotcha. And so that’s why this was such a landmark study was because it opened up conversations into symptom management. It opened up conversations into different pharmacological routines, into alternative pain treatments. Like how Matt Bair is doing this. It seems like this was a really, really big study.
Kurt Kroenke: 10:51
It was really important because first of all they’ll probably never be another study done like that again because the whole issue with opiates, there’s so much less use. So the timing was right and, and the outcomes were important. You alluded to something because this study just focused on pharmacologic medication treatment and showed if you used the right combinations of medicines other than opiates and compared them to opiates on average, you could get about equal pain outcomes potentially with less side effects, but it didn’t study nonpharmacologic treatments. So there was this all evidence for exercise cognitive behavioral therapy, mindfulness based treatments, acupuncture, Yoga, chiropractic, which also have evidence. So probably the take home messages with a person with chronic pain, we should use a combination of the right combination of non-opiate medicines and behavioral nonpharmacologic treatments. And then opiates would have a very small role in the treatment of chronic pain.
Phil Lofton: 11:53
Which raises the question, where does symptom management go with that information?
Kurt Kroenke: 11:57
There’s a couple schools of thought out there. So I think there’s two tracks. Okay. Not, just one track, one track is for the patient who’s a chronic pain, who’s never been on opiates. I think moving forward, only a very small percent of those should ever end up on opiates. And that’s mainly if we’ve appropriately tried a series of others, finding the right combination of medicines and behavioral kinds of treatments. On that track, there are issues of reimbursement and access for behavioral treatments and it takes some time. And so I think in primary care where I work, where there’s not enough pain clinics out there to treat every bit of the pain, we need to find the right kinds of time and primary care and the support for it. We found models of working with nurse care management and telecare. So I think having access to those treatments and having a systems of care, where we can adequately follow the patient.
Kurt Kroenke: 12:57
We need that for the patient who’s never been on opiates, which most patients, we have about five to 10 million Americans with chronic pain on opiates. And they feel a little beleaguered because there’s this big movement to get everybody off. And so they feel they were started in good faith, most don’t abuse. So I have a little different view about if their patients are doing well with this group of patients that we started at opiates often years ago. We shouldn’t immediately pull the plug, we should humanely manage them. A lot of the regulations that have come in have been very sort of onerous because of the addiction problem. So I guess there’s a third track. The third track is the opiate addiction in this country and the opioid addiction in this country largely is a lot of people without chronic pain. It’s a separate problem and that issue is pretty clear.
Kurt Kroenke: 13:49
We have to have good opioid treatment programs. We cannot stigmatize them and there’s a lot of movements going on. So I guess at the end of the day there’s three tracks. So the people who’ve never been on opiates with chronic pain, very few, should end up on opiates. The patients with chronic pain on opiates often for years. We got to be careful about pulling the plug too soon. And third, a somewhat separate issue, is the opiate addiction crisis that we have. And there’s a, that’s another area where policy and, and regulations and reimbursement play a role.
Phil Lofton: 14:26
After the break, we’ll talk to Marianne. Matthias, she’s a health communications researcher working on tapering opioids. Learn how doctors can get patients off of opioids effectively or not. Start them down that path at all. When we return on the problem.
Pathways Ad: 14:40
Approximately 80 percent of people in the United States will hold a phd degree in the biomedical sciences are not tenure track faculty. What jobs do they have and how did they find them? Are they actually using their doctoral education and they’re not academic careers? I’m Randy Rundquist, Associate Dean for research and graduate studies at the Indiana University School of medicine. Welcome to Pathways. Here, we do more than just tell you what nonacademic jobs you could potentially have with a phd in the biomedical sciences. We talked with those who are actually in these positions. What do they do, and most importantly, what was their path to ultimately land their job? Join us as we explore the many possibilities to use your biomedical Phd Degree in a career you perhaps did not even know it was out there. Pathways will take us there.
Phil Lofton: 15:38
Hey, welcome back. So we’ve learned some of the reasons why health communications led to a boom in opioid prescription, and more importantly, we’ve learned that opioids may not be as effective in relieving pain as we might have been led to believe. So what do we do? One of the ways forward is discussed by Marianne Mathias. I sat down with her to talk about her new paper: “I’m not going to pull the rug out from under you”.
Marianne Matthias: 16:01
Well, the paper is about opioid tapering and that actually is a quotation from one of the providers in the study. When in the clinic visit they were tapering the patient and they wanted to make it clear to the patient that they’re not going to abandon them. I’m not going to pull the rug out from under you. So that’s where we got it. We had really three sources of data for that study. We we recorded, we audio recorded primary care visits with patients and their providers, patients who were taking opioids for chronic pain. And then later on we interviewed the patients and then separately we interviewed the providers and from that study we were able to uncover what you might call best practices for communicating about opioid tapering. And we learned from that study that patients really value having some input into the tapering process, even if in a lot of cases these patients were being tapered because they had to be tapered either because of a state law or because of an institutional mandate.
Marianne Matthias: 17:12
So the provider might not have had a choice about tapering, but if patients could be given some input into even like the rate of tapering, how fast their doses go down, patients and providers felt better about it because it gave them some control and some sense of ownership of their own health in their own treatment. Another thing we learned from that study is that patients really needed to know that they weren’t going to be abandoned by their providers. So they needed to know that their providers weren’t just going to cut their opioids and then leave. And we observed a lot of cases both in the clinic visits and in the interviews of providers, especially reassuring their patients, you know, I’m, I’m not leaving, I’m not going anywhere. It’s not going to happen. I’m going to be here with you through the whole time.
Marianne Matthias: 18:06
So those types of things we found were just, they helped facilitate, I think, smoother tapering because the patients really felt supported and they felt like they were, you know, in it with their provider and that they were, they were working as a team instead of it being some kind of adversarial thing where, yep, we’re gonna, we’re gonna decrease your opioids and here’s how it’s going to be. So both feeling like they had some input and feeling like they were supported, I think was really important during the tapering process.
Marianne Matthias: 18:41
I think that even before there was a declared opioid crisis, I think communication about opioids was always perceived to be a little bit difficult by providers. And often my patients, and there are reports from, you know, we’ve done prior research, other people have done research where patients report feeling like they’re being treated like they’re drug addicts, providers report that all they want is opioids, they don’t want to listen to anything else. So it’s been a source of conflict for quite some time.
Marianne Matthias: 19:16
And so I think with the, in some ways the declaration of an opioid crisis, I think based on our latest work, some providers feel like it has, I’m liberated them a little bit and I say that meaning there are now state and oftentimes institutional mandates to reduce opioid doses and to have opioid agreements or some people call them contracts with patients that say things like, I can’t get prescriptions from another provider. You know, they have to follow this set of rules. And so I think in many cases providers feel empowered a little bit more to say no to opioids when they’re asked about them, which before they may have felt like it wasn’t the best option for the patient. But they felt a lot of pressure. Now they, they have the supportive institutions of state laws of the public because it’s so, you know, the opioid crisis is so well known now, so I think it’s been, it’s been helpful in that way.
Marianne Matthias: 20:19
And I think another way that communication plays into this is because sometimes opioids are off the table now as a treatment option, there’s a lot of room for shared decision making, which is an important part of any kind of treatment because if a person can’t have opioids, if they’re or if they’re opioids are being reduced or taken away, they need to find other sources of treatment. And there are, there a lot of options for pain management. There are, you know, complimentary and integrative health options like acupuncture and meditation and things like that, but they’re more traditional options like physical therapy and there are often integrated pain management clinics, but that kind of, that kind of thing needs to be talked out. And the options need to be weighed. Pros and cons needed to be discussed. Some patients, for example, can’t go to physical therapy. Maybe they have transportation issues or they can’t get off work. So all of that requires good communication and negotiation in some cases. So I think that a communication permeates both opioid prescribing and just pain management in general because so much of pain management, whether it’s opioids or not as communication.
Phil Lofton: 21:40
So can we unpack that a little bit? So how has the way that we talk about pain as a society, do you think that’s played any role in the opioid crisis?
Marianne Matthias: 21:50
I think anecdotally in our society maybe is a little bit more averse to pain than maybe other cultures. And I think that if you look at opioid prescribing in European countries for example, they frequently don’t even prescribe opioids after surgery, which is pretty standard in this country. So I think another example is childbirth. Most childbirth in the US is in a hospital setting usually with some kind of pain management. Frequently in European countries as well as other countries. Childbirth is, it happens more frequently outside of the hospital, maybe in a home setting without pain management. Not all the time, but it is more common than in this country. So I think, I think just as a society, we are conditioned to avoid pain when many would argue pain is a part of life.
Marianne Matthias: 22:49
When you’re managing pain, especially in an environment where opioids are seen as presenting more harm than, than probably helping patients, the patient provider relationship is critical and that’s regardless of what the policies are. And it may be especially true when there are policies that demand that opioids be discontinued or not started or reduced, uh, and time after time again and work we’ve done, whether it was focused on opioids or whether it was not focused on opioids and just focused on pain management in general patients really respond well when they feel like they have a provider who genuinely cares about them. We did a study years ago before anybody uses the words opioid crisis and patients responded to provide saying no to opioids or providers decreasing opioids if they proceed, they’ve responded well to that. If they perceived that their providers were doing it out of genuine concern for their health, that they were on the same team as opposed to their providers feeling adversarial. Like, I think you’re a drug addict or I can’t prescribe this to you, I’m endangering my license. So when they felt that alliance, that bond with their provider and felt like they were really playing on the same team, then it gave a lot. It gave providers a lot more latitude in terms of what they could discuss with patients because again, patients knew that they were looking out, their provider was looking out for them and their best interests.
Phil Lofton: 24:38
So with regards to tapering and to pain management, a developed attentive relationship, it makes a world of difference. True honest communication helps doctors provide effective care. Join us next time when we talk about community health, a field of boots on the ground health workers that’s built on communication just like this.
Music in this episode is by Everlone with an additional sound collage by the central state singers. Our theme and additional musical cues were written and performed as always by Mississippi’s own, Eldon O’Shaughnessy and the down and out quartet. The problem is produced at studio 132 in the Regenstrief Institute in Indianapolis, Indiana where we connect and innovate to provide better care and better health. Learn more about our work and how you can get involved at regenstrief.org And see bonus content from this episode including sources, pictures and more at regenstrief.org/theproblem.